By Marina Townsley
Have you ever made a decision following your ‘gut feeling’? Or had ‘butterflies in your stomach’ before an interview or exam? Or had an upsetting ‘gut wrenching’ experience? Few of us realise that in many life situations we are getting messages from our ‘second brain’, which is hidden in our bowels and is called the Enteric Nervous System (ENS). The truth is that our brain and our gastrointestinal system are intimately connected, and the importance of a healthy gut microbiome has huge implications for your overall health.

What is the Gut-Brain Axis?
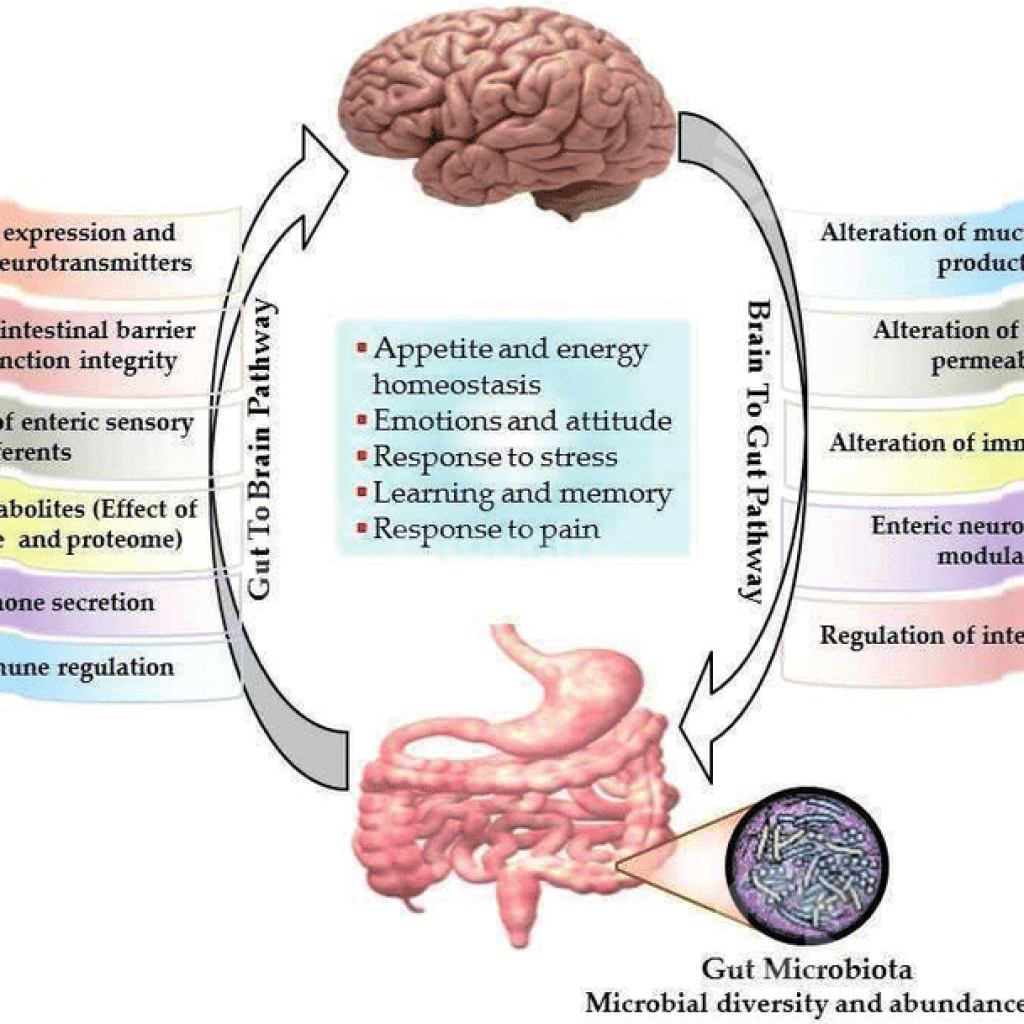
It is a two-way biochemical communication system that connects our brain (Central Nervous System or CNS) and our gut, so that a distressed brain can send messages to the gut and a distressed gut can send message to the brain. The third very important participant of this physiological conversation is the bacteria (microbiota) that reside in your gut, making it the Gut-Microbiota-Brain Axis.
How do the brain and the gut communicate?
The brain and the gut ‘talk’ to each other via two thin layers of more than 100 million nerve cells lining your gastrointestinal tract, neurotransmitters, inflammatory cytokines, neuropeptides, local hormones and antibodies produced in the gut wall. Although the ENS is not capable of ‘thought’ as we understand it, and governs autonomic processes like digestion, appetite, gut motility, nutrient absorption, production and turnover of neurotransmitters, gut hormones and mucus secretion, local immune defences against pathogens, at the same time it is very sensitive to emotions and can influence memory, cognition and mental health.
Do mood disorders cause gut problems or the other way round?
Medical professionals previously thought that anxiety and depression cause functional digestive disorders like Irritable Bowel Syndrome (IBS), but the latest studies show that abdominal pain, bloating, spasms, constipation, diarrhoea or dysbiosis in the gut that causes irritation and inflammation may send a signal to the brain that can trigger mood changes. It becomes a ‘chicken and egg’ situation, where embarrassing gastrointestinal symptoms may cause anxiety and stress, but worry, stress or fear can often trigger uncomfortable gastrointestinal symptoms too. In other words, intestinal distress can be both a product and a cause of high stress, depression or anxiety.
What’s the connection between stress and the gut?
The multiple connections within the Gut-Brain Axis incorporate the Vagus nerve, the immune and endocrine signalling systems like the HPA axis (Hypothalamus-Pituitary-Adrenal Axis, which is our stress response system) as well as bacterial metabolites from the gut microbiome. We now know that stress can alter the composition of the gut microbiome, making it less diverse and more susceptible to harmful bacteria, increasing immune inflammatory response, leading to increased gut permeability (‘leaky gut’), food sensitivities, breach of the blood-brain barrier and adverse effects of bacterial metabolites on the brain. Gut dysbiosis (adversely altered gut microbiome composition) is linked to a variety of brain-related and systemic disorders ranging from depression and anxiety to Parkinson’s and Alzheimer’s diseases, MS and autism.
How does the gut microbiome affect brain function?
The gut microbiota can produce a range of neurotransmitters, hormones and neuroactive substances like acetylcholine, catecholamines, gamma-aminobutyric acid, histamine, melatonin and serotonin (90% of which is produced in the gut rather than the brain); all of these are essential for regulating peristalsis and sensation in the gut. Changes in the composition of the gut microbiota due to diet, medication, chronic stress or disease will lead to changes in the levels of circulating cytokines, some of which can affect brain function. The gut microbiota can directly activate the Vagus nerve, which transmits information about the state of the intestines to the brain.
How can you tell if you have dysbiosis?
Our daily bowel motions can provide some valuable insight into the health of our digestive system. Acid reflux, constipation, bloating, diarrhoea, fatigue may be signs of gut dysbiosis or other gastrointestinal problems. They could be further explored with detailed functional medicine tests, which analyse stool, blood, urine and saliva, and provide a good road map to the necessary treatment, dietary and lifestyle changes.
Is diet important for Gut-Brain Axis health?
Diet plays a crucial role in gut microbiome health as it provides prebiotic fibre, complex carbohydrates and other food for our gut bacteria. They in turn produce short chain fatty acids and other substances that nourish and repair our gut, the whole spectrum of B-vitamins including biotin, cobalamin, folate, niacin, pantothenate, pyridoxine, riboflavin and thiamine, some of which are necessary for central nervous system function like B12, and the others for energy production, liver detoxification pathways, hormone regulation and other metabolic functions. As previously mentioned, our gut bacteria also produce a range of neurotransmitters that directly affect our mood. Feeding our little friends in the gut with varied and nutritious diet pays off as balanced and healthy gut microbiome benefits us in so many ways.
Are antibiotics the only way to treat dysbiosis and minor infections?
The overuse of antibiotics can affect the gut and systemic health in a profound way. The latest research suggests that early and frequent exposures to antibiotics may induce autoimmunity and psychiatric illness. There are, of course, certain situations when antibiotic prescription is totally justified and saves lives, but in other situations throat gargles, steam inhalations with essential oils, local use of hydrogen peroxide or iodine may eliminate infections without antibiotics. They kill off our friendly gut bacteria that protect us from pathogenic organisms and constitute a major part of our natural immune defences; encourage proliferation of antibiotic-resistant bacterial strains; often cause diarrhoea and adversely affect our central nervous system causing mood dysregulation.
What can you do to support a healthy Gut-Brain Axis?
What therapies and interventions can help both gut and brain issues?
Nutritional Therapy can help to select the best diet for you as well as to establish any nutritional deficiencies, food triggers that irritate the gut, cause immune reactions or feed the wrong types of bacteria and yeasts in the body. Nutritional supplements can be effective therapeutic solutions in some situations to support certain metabolic pathways and provide nutrients that support brain function.
Functional Medicine can offer very advanced tests, which will provide valuable insights into the causes of your gastrointestinal and/ or brain-related conditions. This information then enables your therapist or medical practitioner to treat the cause of the problem. Examples might be heavy metals, mould toxicity, neuroendocrine or gut microbiome testing. There are new sophisticated tests from Dr. Dale Bredesen, who developed his own treatment protocols for addressing dementia, Alzheimer’s disease and other disorders affecting the brain. Most of them are based on corrected nutrition, specific supplementation and detoxification procedures.
Herbal Medicine comes to the rescue where pharmaceuticals are not well tolerated or gentler treatment methods are required. Medicinal herbs are usually better tolerated and they an advantage in that they have not been overused, so bacteria have not developed tolerance to them. Herbs are better recognised and used by the body because they come somewhere between foods and drugs, and they contain biologically active substances that are not totally foreign to our bodies.
Frequency Specific Microcurrent is a fairly new and promising electromagnetic therapy, which works directly on the brain, nervous tissue, the Vagus but can also be successfully applied to abdominal organs to treat various pathogens, dissolve scar tissue and adhesions, improve gut motility and liver function. The current is very low (at the physiological level like nerve impulses) and therefore not felt at all usually. There are two channels, one of which is aimed at a particular tissue and the other at the state of that tissue. The frequencies used are specific for different target tissues and organs, and different pathological conditions. The results are reproducible and this treatment modality is becoming increasingly popular with the mainstream medical community in the USA, Australia and Germany. Sutherland House is a London based multidisciplinary clinic where the majority of practitioners are trained in FSM.
References:
1. Marilia Carabotti, Annunziata Scirocco, Carola Severi. The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol 2015 Apr-Jun;28(2):203-209.
2. Foster JA, McVey Neufeld KA. Gut-brain axis: how the microbiome influences anxiety and depression. Trends Neurosci. 2013;36:305–312.
3. Mayer EA, Savidge T, Shulman RJ. Brain-gut microbiome interactions and functional bowel disorders. Gastroenterology. 2014;146:1500–1512.
4. Hillestad EMR, van der Meeren A, Nagaraja BH, Bjørsvik BR, Haleem N, Benitez-Paez A, Sanz Y, Hausken T, Lied GA, Lundervold A, Berentsen B. Gut bless you: The microbiota-gut-brain axis in irritable bowel syndrome. World J Gastroenterol. 2022 Jan 28;28(4):412-431. doi:10.3748/wjg.v28.i4.412.
5. Francisco Javier Díaz-García, Saúl Flores-Medina, Diana Mercedes Soriano-Becerril. Interplay between Human Intestinal Microbiota and Gut-to-Brain Axis: Relationship with Autism Spectrum Disorders. Nov 2019; doi:10.5772/intechopen.89998
6. Andrina Rutsch, Johan B. Kantsjo, Francesca Ronchi. The Gut-Brain Axis: How Microbiota and Host Inflammasome Influence Brain Physiology and Pathology. Front. Immunol., 2020 Dec 10;
Sec. Multiple Sclerosis and Neuroimmunology, vol.11 https://doi.org/10.3389/fimmu.2020.604179
7. Petra, AI; et al. Gut-Microbiota-Brain Axis and Its Effect on Neuropsychiatric Disorders With Suspected Immune Dysregulation. Clin. Ther.37(5): 984 -95. May 2015. doi:10.1016/j.clinthera.2015.04.002.
8. Jeremy Appleton, ND. The Gut-Brain Axis: Influence of Microbiota on Mood and Mental Health. Integr Med (Encinitas). 2018 Aug; 17(4): 28–32.
Marina Townsley
Naturopath ND, Nutritional Therapist BANT
Master Herbalist AMH
Advanced FSM Practitioner