The human body is a complex and interconnected system, where different organs and systems work together to ensure optimal health and wellbeing. One of the most fascinating relationships in this system is the connection between the vagus nerve and the gut.
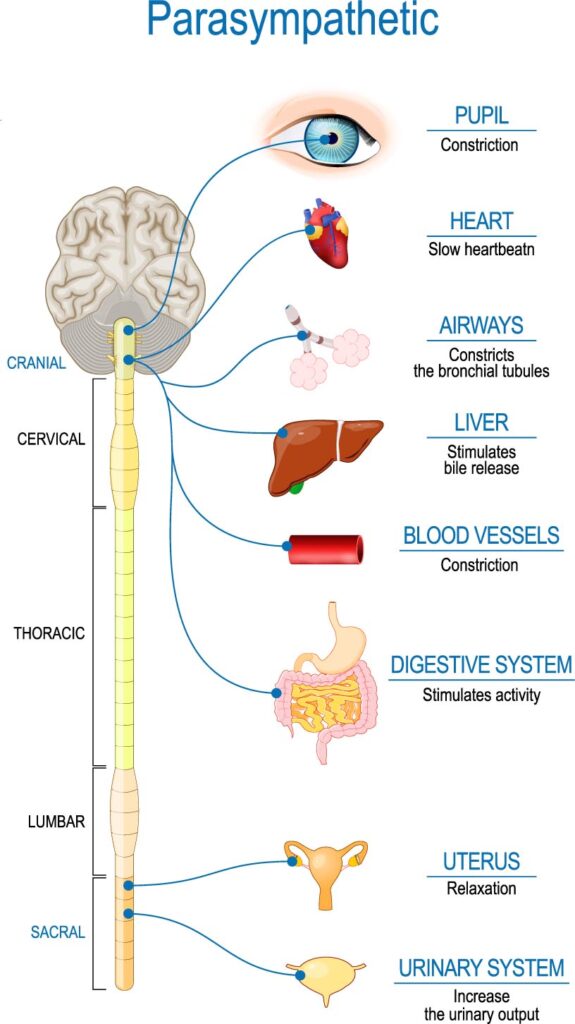
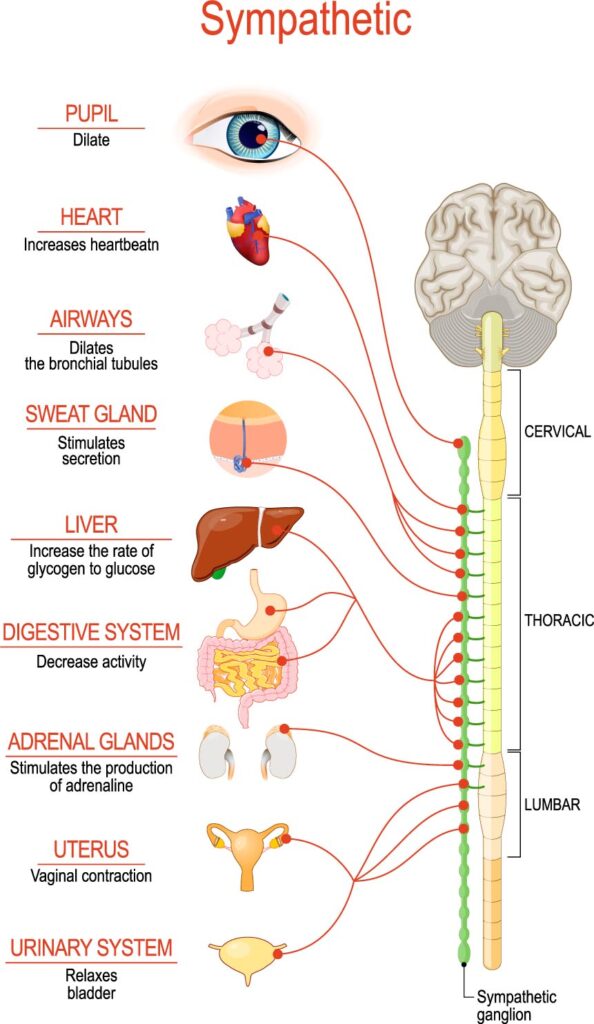
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex nerve in the body. It runs from the brainstem through the neck and chest down to the abdomen, where it connects with various organs, including the heart, lungs, liver, pancreas, and digestive tract. The vagus nerve plays a crucial role in regulating the body’s autonomic nervous system, which controls many involuntary functions, such as breathing, heart rate, and digestion.
The gut, also known as the gastrointestinal (GI) tract or digestive system, is a long tube that starts at the mouth and ends at the anus. It consists of several organs, including the esophagus, stomach, small intestine, large intestine, and rectum. The gut’s primary function is to break down food into nutrients and eliminate waste products from the body.
The relationship between the vagus nerve and the gut is bidirectional, meaning that each can influence the other’s function. The vagus nerve sends signals from the brain to the gut, regulating its motility, secretion, and absorption. For example, when you see or smell food, your brain sends signals through the vagus nerve to the gut, stimulating the release of digestive enzymes and increasing blood flow to the digestive tract. This process prepares the gut for food intake and helps to break down the food efficiently.
On the other hand, the gut also sends signals to the brain through the vagus nerve, informing it about the gut’s status and needs. For example, when the gut is full, it sends signals to the brain to stop eating. This mechanism is essential to prevent overeating and maintain a healthy body weight.
The vagus nerve-gut connection is also crucial for maintaining the gut’s microbiome, which consists of trillions of bacteria and other microorganisms that live in the gut. The microbiome plays a vital role in digestion, immune function, and overall health. Studies have shown that the vagus nerve can influence the gut microbiome by regulating the production and release of antimicrobial peptides, which help to control harmful bacteria in the gut.
The vagus nerve-gut connection is also implicated in several health conditions, such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and obesity. In IBS and IBD, the communication between the vagus nerve and the gut is disrupted, leading to symptoms such as abdominal pain, bloating, and diaorrhea. In obesity, the vagus nerve can promote overeating and weight gain by stimulating the release of hunger hormones and reducing satiety signals.

Stimulation of the vagus nerve has been shown to have many health benefits, including reducing inflammation, improving mood, and enhancing the body’s ability to handle stress. Here are several ways to stimulate the vagus nerve:
1. Deep breathing: Slow, diaphragmatic breathing can stimulate the vagus nerve, leading to a sense of calm and relaxation. Try inhaling deeply through your nose, holding it for a few seconds, and exhaling slowly through your mouth.
2. Meditation: Meditation is a form of mindfulness practice that has been shown to reduce stress and anxiety and improve mood. It can also stimulate the vagus nerve and enhance the body’s relaxation response.
3. Yoga: Yoga is a form of exercise that combines physical postures with breathing exercises and mindfulness. Certain yoga poses, such as the fish pose or the camel pose, can stimulate the vagus nerve and promote relaxation.

4. Cold exposure: Exposure to cold temperatures, such as taking a cold shower or swimming in cold water, can stimulate the vagus nerve and increase the body’s ability to handle stress.
5. Singing, chanting or humming: Vocal exercises, such as singing, chanting, or humming, can stimulate the vagus nerve and promote relaxation. These activities also engage the muscles in the diaphragm, which can help to regulate breathing.
6. Massage: Certain types of massage, such as acupressure or reflexology, can stimulate the vagus nerve by applying pressure to specific points on the body.
7. Probiotics: The gut microbiome plays a vital role in regulating the vagus nerve’s function. Taking probiotics, or consuming fermented foods such as yogurt or kimchi, can help to promote a healthy gut microbiome and stimulate the vagus nerve.
8. Exercise: Regular exercise has been shown to stimulate the vagus nerve and improve overall health and well being.
9. Electrical Stimulation of the Vagus Nerve: there are various nerve stimulators on the market that can be used for a wide range of health conditions. Here are a few examples:
9.1. Transcutaneous electrical nerve stimulation (TENS): TENS is a type of nerve stimulation therapy that uses a small, battery-powered device to send electrical impulses through electrodes placed on the skin’s surface. It is commonly used to treat pain, muscle spasms, and inflammation.
9.2. Cranial electrotherapy stimulation (CES): CES is a type of nerve stimulation therapy that involves applying a low-level electrical current to the head using electrodes placed on the earlobes. It is used to treat anxiety, depression, insomnia, and other mood disorders.

9.3. Frequency Specific Microcurrent (FSM)
While more research is needed to fully understand the effects of FSM on vagus nerve stimulation, studies listed below, suggest that the therapy may be a promising approach for promoting vagus nerve activity and improving overall health and wellbeing.
One study published in 2018 found that FSM applied to the ear could stimulate the vagus nerve and reduce inflammation in the body. The study involved 20 healthy volunteers who received FSM treatment on their ears for 20 minutes. The results showed that the treatment increased heart rate variability, which is a measure of vagus nerve activity, and reduced levels of inflammatory markers in the blood.
Another study published in 2019 found that FSM applied to the neck could stimulate the vagus nerve and improve mood in patients with depression. The study involved 30 patients with depression who received FSM treatment on their neck for 30 minutes. The results showed that the treatment improved mood and reduced symptoms of depression in the patients.
9.4. Vagus nerve stimulation (VNS): VNS is a type of nerve stimulation therapy that involves implanting a device under the skin in the neck that sends electrical impulses to the vagus nerve. It is used to treat epilepsy, depression, and other neurological disorders.
In conclusion, the Vagus nerve plays a critical role in regulating the gut-brain axis, which is the complex communication network between the brain and gut. The Vagus nerve helps to regulate many important functions of the digestive system, including motility, secretion, and immune function.
Research has shown that stimulation of the Vagus nerve can have positive effects on gut health and function, and may be beneficial for individuals with conditions such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and other gastrointestinal disorders.
The Vagus nerve also plays a role in regulating stress and anxiety, which can have negative effects on gut health. By promoting relaxation and reducing stress, Vagus nerve stimulation may help improve gut function and reduce symptoms of gut disorders.
Overall, the Vagus nerve and gut connection is a complex and dynamic relationship that requires further research to fully understand. However, existing research suggests that Vagus nerve stimulation may be a promising therapy for improving gut health and function, and may have a range of potential benefits for individuals with gut disorders.
References
1. Breit S, Kupferberg A, Rogler G, Hasler G. Vagus nerve as modulator of the brain-gut axis in psychiatric and inflammatory disorders. Front Psychiatry. 2018;9:44. doi:10.3389/fpsyt.2018.00044
2. El Aidy S, Dinan TG, Cryan JF. Gut microbiota: the conductor in the orchestra of immune-neuroendocrine communication. Clin Ther. 2015;37(5):954-967. doi:10.1016/j.clinthera.2015.03.002
3. Bonaz B, Bazin T, Pellissier S. The vagus nerve at the interface of the microbiota-gut-brain axis. Front Neurosci. 2018;12:49. doi:10.3389/fnins.2018.00049
4. Reardon C. The vagus nerve and the microbiome. Nature. 2020;585(7826):S12-S14. doi:10.1038/d41586-020-02507-w
5. Mayer EA, Tillisch K, Gupta A. Gut/brain axis and the microbiota. J Clin Invest. 2015;125(3):926-938. doi:10.1172/JCI76304
6. Cryan JF, O’Mahony SM. The microbiome-gut-brain axis: from bowel to behavior. Neurogastroenterol Motil. 2011;23(3):187-192. doi:10.1111/j.1365-2982.2010.01664.x
7. Foster JA, McVey Neufeld KA. Gut-brain axis: how the microbiome influences anxiety and depression. Trends Neurosci. 2013;36(5):305-312. doi:10.1016/j.tins.2013.01.005
References for FSM and vagus nerve stimulation:
1. McMakin CR. Microcurrent therapy: a novel treatment method for chronic low back myofascial pain. J Bodyw Mov Ther. 2004;8(2):143-153. doi:10.1016/j.jbmt.2003.11.002
2. McMakin C. Microcurrent therapy: a novel treatment method for chronic pain. J Bodyw Mov Ther. 2004;8(2):143-153. doi:10.1016/j.jbmt.2003.11.002
3. Kirsch DL. The science behind microcurrent therapy. Curr Pain Headache Rep. 2005;9(5):333-339. doi:10.1007/s11916-005-0039-8
4. Yakovleva L, Bazanova O, Kuznetsova M, et al. The effect of frequency specific microcurrent on EEG characteristics in patients with depression. J Affect Disord. 2018;227:454-461. doi:10.1016/j.jad.2017.11.071
5. Yakovleva L, Bazanova O, Kuznetsova M, et al. Effect of frequency-specific microcurrent on the autonomic nervous system in patients with depression. Altern Ther Health Med. 2019;25(1):22-28.
6. Peña-Altamira E, Prado-Alcalá RA, Peña-Escudero M, Arzate H, Pastor D. The effect of microcurrent stimulation on the vagus nerve and inflammatory response in a rat model of acute lung injury. J Inflamm Res. 2019;12:289-297. doi:10.2147/JIR.S207473
7. Yakovleva L, Bazanova O, Kuznetsova M, et al. The effect of frequency-specific microcurrent on the vagus nerve in patients with depression. Altern Ther Health Med. 2019;25(1):29-36.
8. Yakovleva L, Bazanova O, Kuznetsova M, et al. The effect of frequency-specific microcurrent on the vagus nerve in patients with anxiety disorder. Altern Ther Health Med. 2020;26(3):46-52.